Knee Pain Explained
It can be hard to describe exactly where your knee hurts. In this article, Dr. Aleto explains what different areas of knee pain may indicate.
It can be hard to describe exactly where your knee hurts. In this article, Dr. Aleto explains what different areas of knee pain may indicate.
Patients with knee pain can present a variety of symptoms, as well as experience pain in different locations. As we age, the most common cause of chronic knee pain is degenerative arthritis. Degenerative or osteoarthritis can occur in any joint, but most commonly occurs in the knee. No matter the cause of arthritis, the result is the wear of the cartilage that lines the joint. This is a chronic and progressive disease that results in increasing pain and limitations.
Many patients with knee pain have a hard time describing where exactly their pain is and thus often describe general pain all over the joint. However, depending on the pattern of arthritis, the pain may be coming from a specific area of the knee.
When we evaluate knee pain, we generally break the knee into 3 sections: the front (anterior or patellofemoral), inside (medial), or outside (lateral). Often times with degenerative arthritis, one section will wear more significantly than the others (see illustrations below). If the wear is primarily on the inside section, patients can experience more isolated pain on the inside of their knee. Likewise, the outside of the knee can also wear down resulting in outer knee pain.


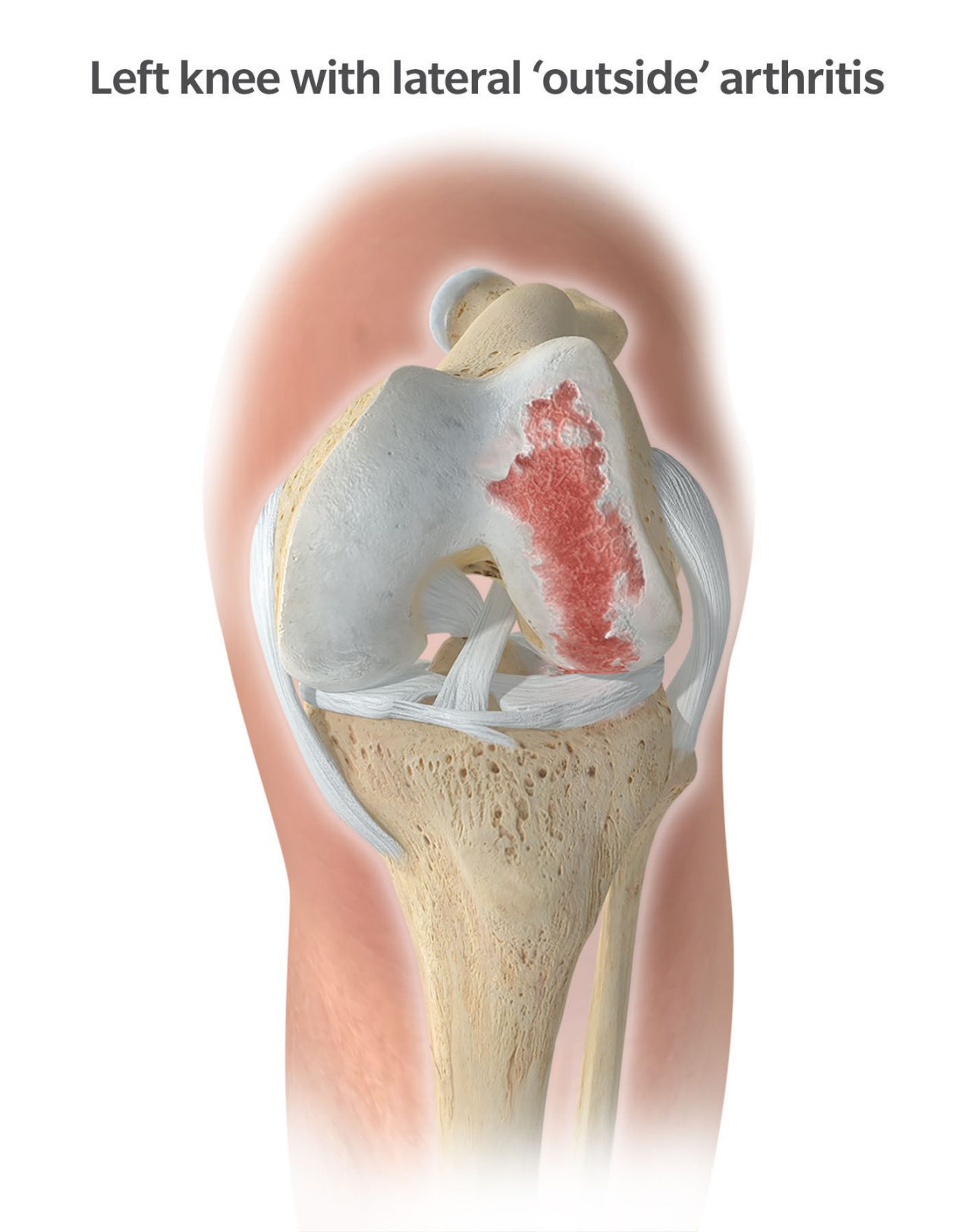

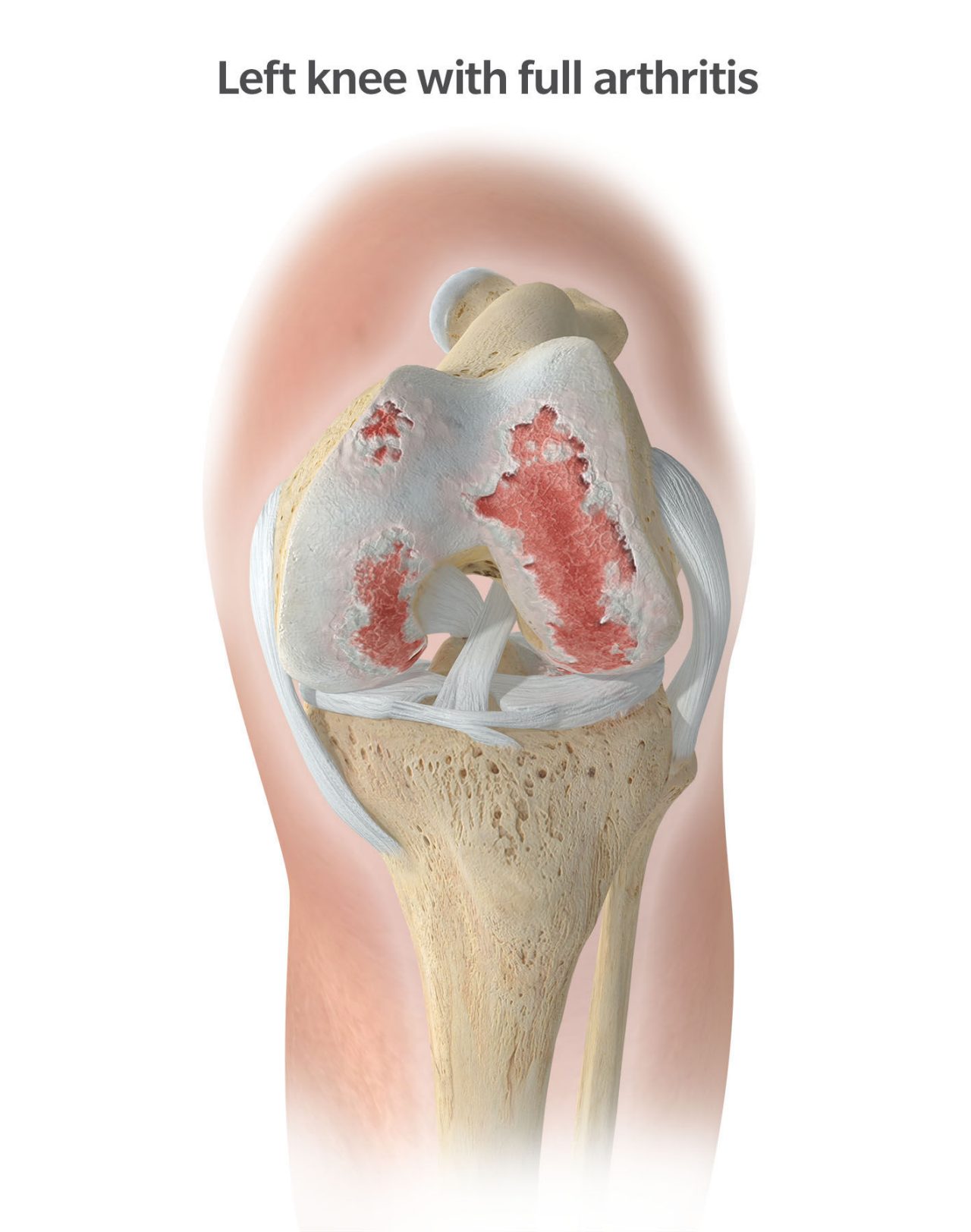
With each of these patterns, as the wear in the joint becomes more severe, patients will often report a progressive deformity about the knee. When the inside wears, patients develop a varus deformity and become bowlegged. When the outside wears, patients develop a valgus deformity and become knock kneed. Isolated wear of the front of the knee is the least common pattern of knee arthritis. These patients generally report pain in the front of their knee that’s worse with squatting, kneeling, and climbing stairs.
 Normal
Normal
 Bowleg
Bowleg
 Knock knee
Knock knee
In addition, many patients report knee swelling that worsens with activity. The swelling, also called effusion, is a result of joint inflammation. The lining of the knee naturally makes synovial fluid to lubricate the joint. With advanced arthritis, the synovial lining becomes inflamed, resulting in increased production of synovial fluid. Patients often describe this swelling in the knee as tightness, difficulty bending, or as a pain/fullness in the back of the knee. This same inflammatory response is what can cause stiffness, achiness, and pain at night. Since many symptoms associated with degenerative arthritis are related to inflammation, anti-inflammatory medications are most commonly prescribed to treat this particular condition.
Given that degenerative or osteoarthritis is truly a wearing-down process, patients often report mechanical symptoms. It’s common for patients to report increased pain when twisting or pivoting due to the bone-on-bone contact that occurs with end-stage progression. Patients can also report popping, catching, and locking as the worn cartilage surfaces deteriorate and fragment. An overall instable feeling may also develop as the knee wears and many patients will report buckling or the knee giving out as a result.
Knee osteoarthritis is evaluated with clinical exam and X-ray evaluations. MRI scans are generally not necessary unless there’s been an injury to the knee. Treatment is determined based upon the severity of your pain and daily imitations. Conservative treatment is recommended initially in all cases. This could include activity modifications, weight loss, anti-inflammatory medications, bracing, therapy, and injections. In patients who don’t find relief using conservative treatments, knee replacement may be an option. But knee replacement surgery comes with risks and is only indicated for end stage, “bone-on-bone” arthritis.
Though arthritic pain is common, there are many other potential sources of knee pain. The presenting signs and symptoms, as well as the location in which they occur are often helpful in determining the source of pain. Traumatic injury can result in ligament injury, tendon disruption, meniscal tears, or even fracture. These injuries are commonly related to a fall or twisting injury to the knee. Given their traumatic nature, they often present with acute onset swelling and inability to bear weight. However, in less severe cases, they may present down the road with continued pain, swelling, instability, and other mechanical symptoms in the knee.
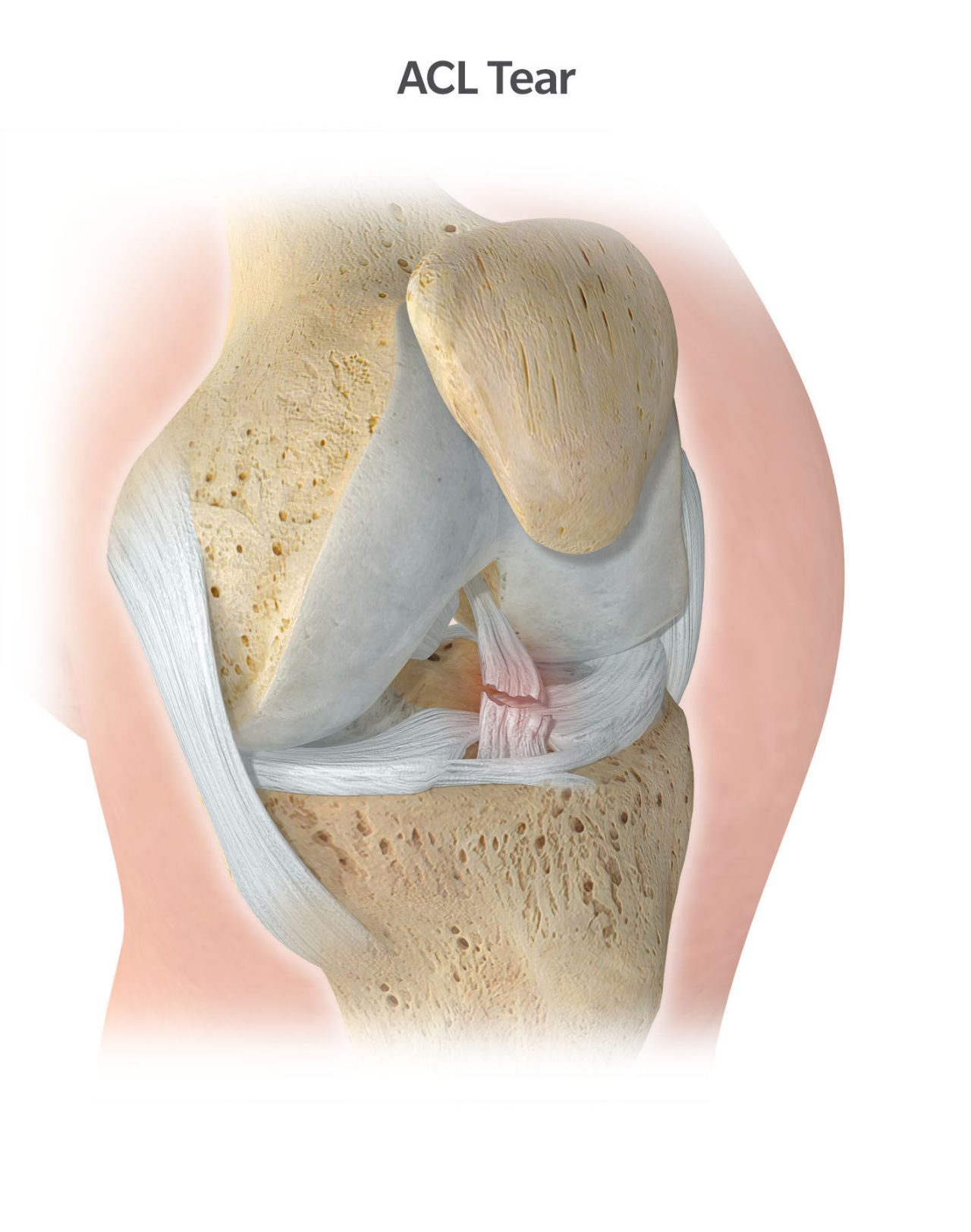
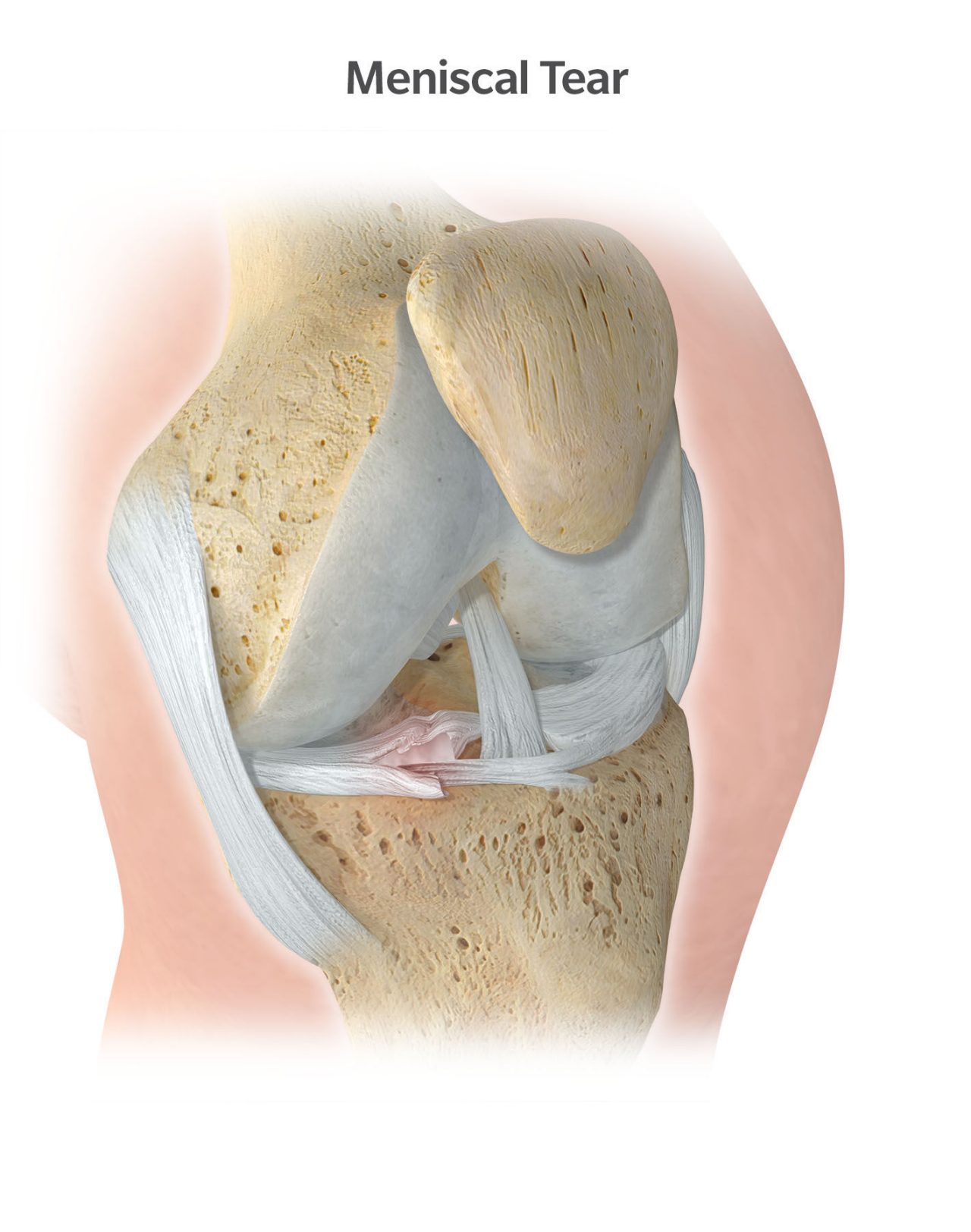
A torn ACL is one of the most common ligament injuries that occur. The ACL is essential in providing stability to the knee joint. Thus, the predominant complaint in these patients is instability, which is typically described as the knee giving out or buckling with activity. Isolated inside or outside knee pain, combined with mechanical catching or locking is commonly seen with meniscal tears.
As with any other source of knee pain, the initial evaluation includes a physical examination of the knee and standard X-rays to rule out an associated fracture. Because these injuries are soft tissue based, i.e. ligament or tendon, an MRI of the knee is commonly required for further evaluation.
Repetitive or overuse injuries are another common source of knee pain. These are frequently referred to as a tendonitis or bursitis. IT band syndrome, pes bursitis, and prepatellar bursitis or “jumpers knee” are all commonly seen conditions as well. These typically present with a history of excessive activity such as walking, running, jumping, or squatting. For many patients, there isn’t a history of acute trauma or injury. These are repetitive injuries that result from micro injury to the ligaments and tendons that provide stability and muscle support to the knee. Patients that are at particular risk are those who have recently begun a new training or exercise program. As a result, many exercise programs recommend a gradual, slow increase in your training to avoid these types of overuse injuries. Given that these conditions are generally inflammatory in nature, they’re usually responsive to conservative management such as activity modifications, physical therapy, and anti-inflammatory medications.