Anatomic vs. Reverse Shoulder Replacements - What are the Differences?
If you’re considering shoulder replacement surgery, you may wonder what the difference is between an anatomic or reverse replacement. In this article, Dr. Sperling explains both.
If you’re considering shoulder replacement surgery, you may wonder what the difference is between an anatomic or reverse replacement. In this article, Dr. Sperling explains both.
If you’ve been told that you may be a candidate for shoulder replacement surgery, you may have been reading about the potential options. Shoulder arthritis tends to be very disabling and can interfere with sleep as well as activities of daily living. You may have heard about anatomic shoulder replacement as well as reverse shoulder replacement; however, the language describing them can be confusing. The purpose of this article is to outline the differences between the procedures and when one procedure may be preferred over the other procedure.
Remember as you research shoulder replacement options, that with any surgical procedure there can be associated risks and complications. Be sure to discuss these with your surgeon. You can also read about some of them by clicking here.
A healthy shoulder without arthritis has smooth motion because the top of the humeral head (ball) and the glenoid (socket) have cartilage covering their surfaces (see “Healthy left shoulder” below). In the case of arthritis, the cartilage is worn resulting in rough surfaces (see “Arthritic left shoulder” below).

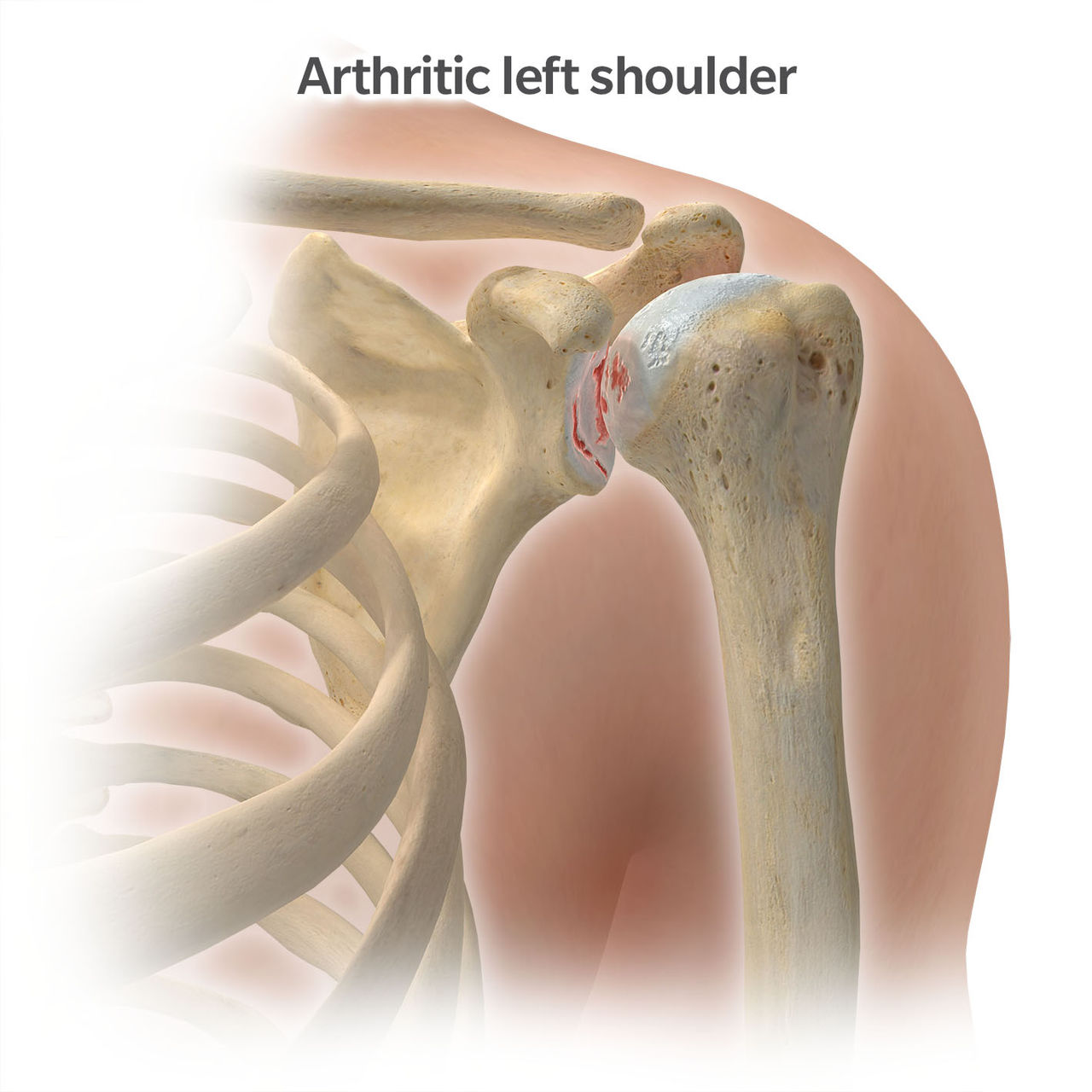
The most common type of shoulder arthritis is called osteoarthritis and typically involves wear of both the ball and socket surfaces. Most patients feel, and sometimes even hear, grinding in the shoulder joint with it catching and clicking. There are some less frequently occurring types of shoulder arthritis such as avascular necrosis where a portion of the humeral head may collapse. In these cases, the arthritis may be isolated to the humeral head ball and not involve the socket.
The rotator cuff is a series of four muscles that connect into the upper part of the humerus. These four muscles are the subscapularis, supraspinatus, infraspinatus, and teres minor. Each of these rotator cuff muscles are composed of a muscle belly that then transitions into a tendon that attaches to the upper part of the humeral bone. The rotator cuff is extremely important for the stability and strength of your shoulder.

Anatomic shoulder replacement is indicated for patients with arthritis in the shoulder and when the rotator cuff muscles are intact or repairable. Anatomic shoulder replacement procedures can be divided into two types:
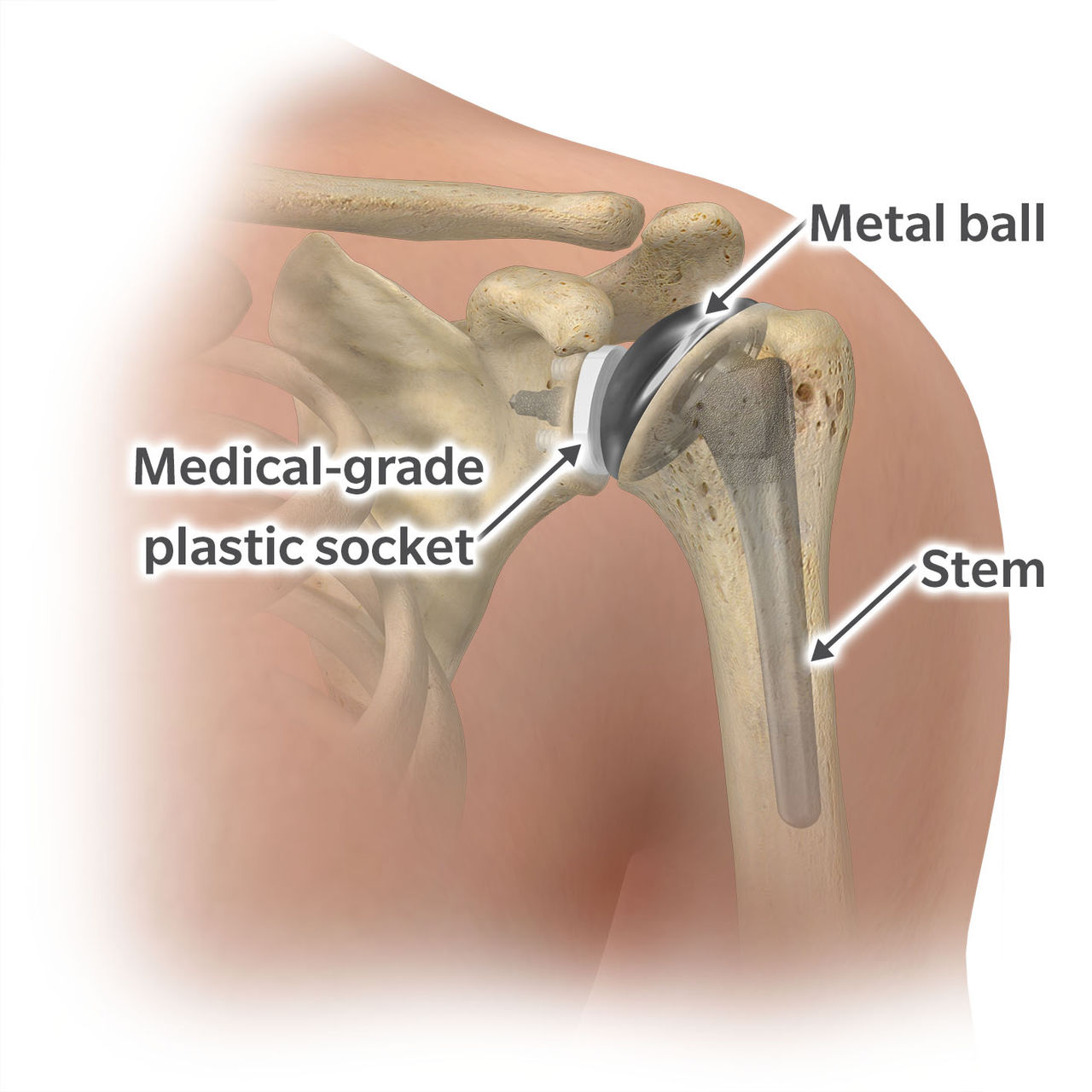
Weight lifting restrictions for the anatomic total shoulder vary among surgeons. Many surgeons have a lifetime weight limit such as 25 pounds with the operative shoulder. Some patients whose recreational activities or occupations require a high weight limit may choose to have a hemiarthroplasty done where there are generally less restrictions.
Results and functional outcomes can vary between hemiarthroplasty and total anatomic replacement and it’s important to talk to your doctor to assess which option can best address your pain and motion. If you do heavy lifting, it’s important to have a discussion with your surgeon in regard to the specific limitations after an anatomic total shoulder replacement compared to a hemiarthroplasty.
In my professional opinion, reverse shoulder replacement represents one of the greatest innovations in orthopedic surgery. Originally developed in Europe in the 1990s, reverse shoulders have been used in the United States for almost twenty years. Originally used for patients with non-repairable rotator cuff tears and shoulder arthritis, the indications have broadened significantly over time. Some of the indications for a reverse shoulder include shoulder arthritis with a non-repairable rotator cuff tear, a massive rotator cuff tear without arthritis, select shoulder fractures, shoulder arthritis associated with a large amount of glenoid (socket) bone loss, instability of the joint surface, and revision cases.
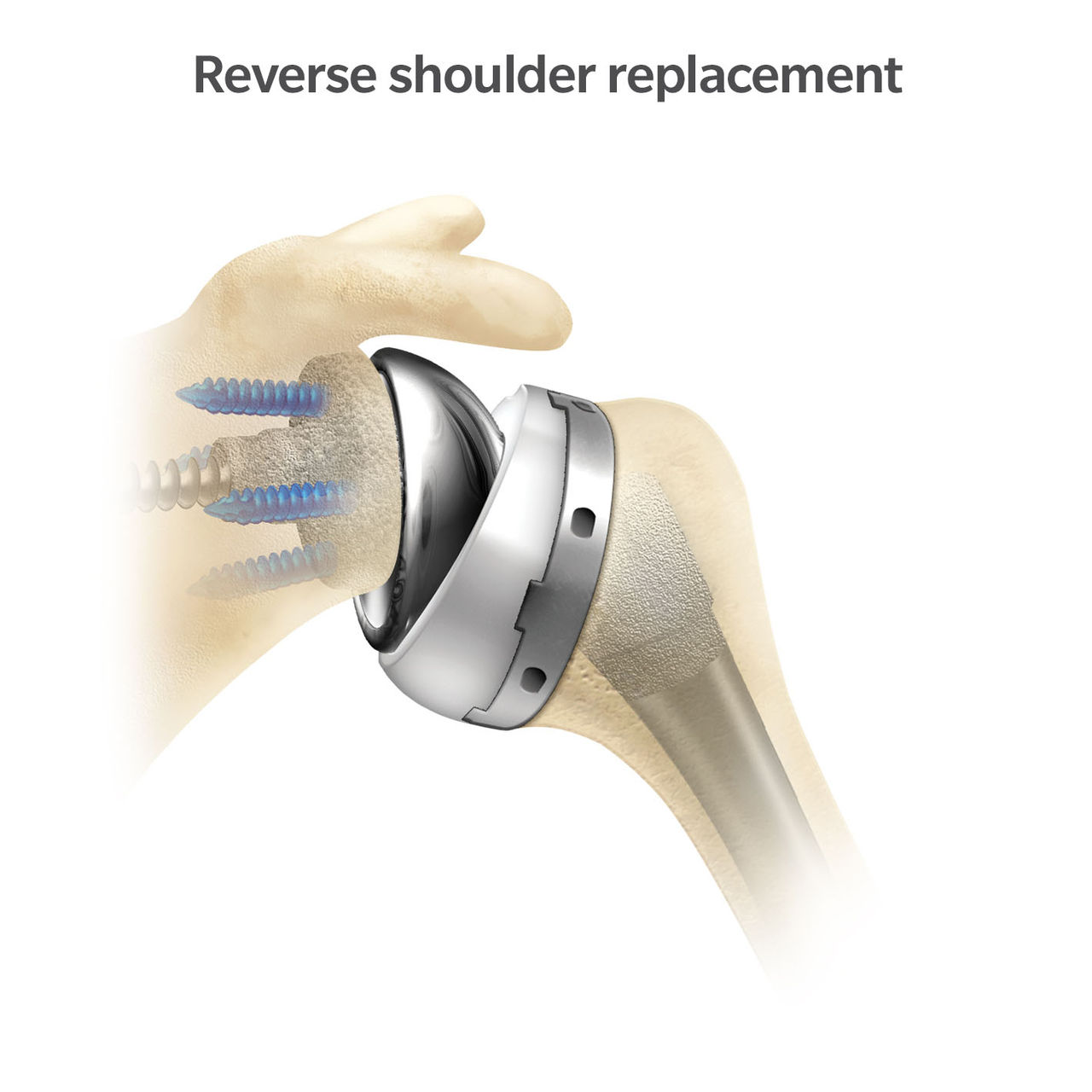
In a reverse shoulder, a small metal baseplate is attached to the glenoid (socket) with medical screws. This metal baseplate is coated with a special material that allows bone to grow into the implant which is how it stays attached in the long-term. Compared to an anatomic shoulder replacement where cement is routinely used to attach the glenoid (socket) implant, in a reverse replacement cement is not used on this socket implant. After the metal baseplate is in place, a round sphere, called a glenosphere, is inserted onto it. This makes the socket side, which used to be “cup” shaped, now round.
The below two images are edited to illustrate the differences between the anatomic and reverse shoulder implants. In reality, the implants shouldn’t have a gap between them. The left image shows the anatomic shoulder implanted; on the right shows the reverse shoulder implanted.
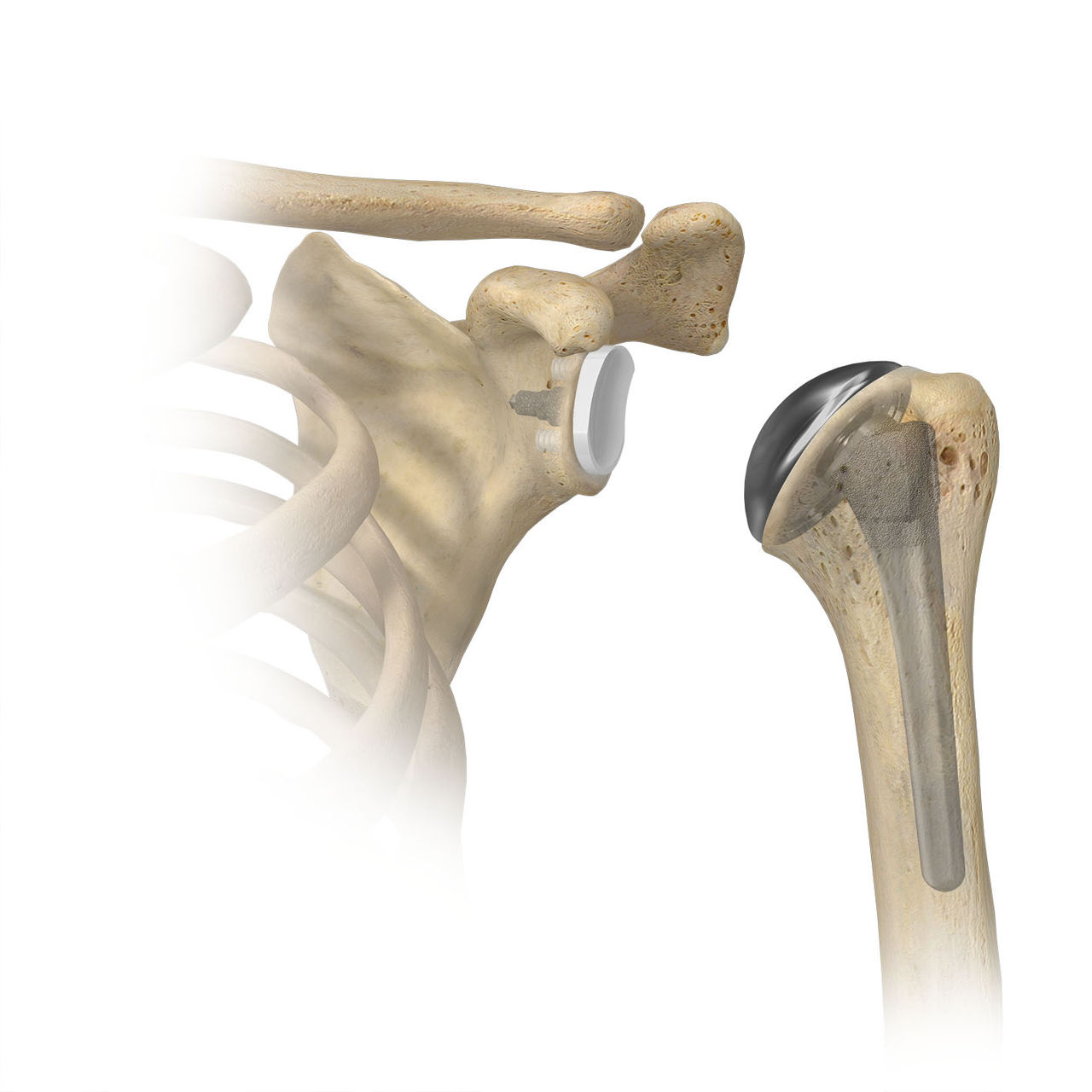
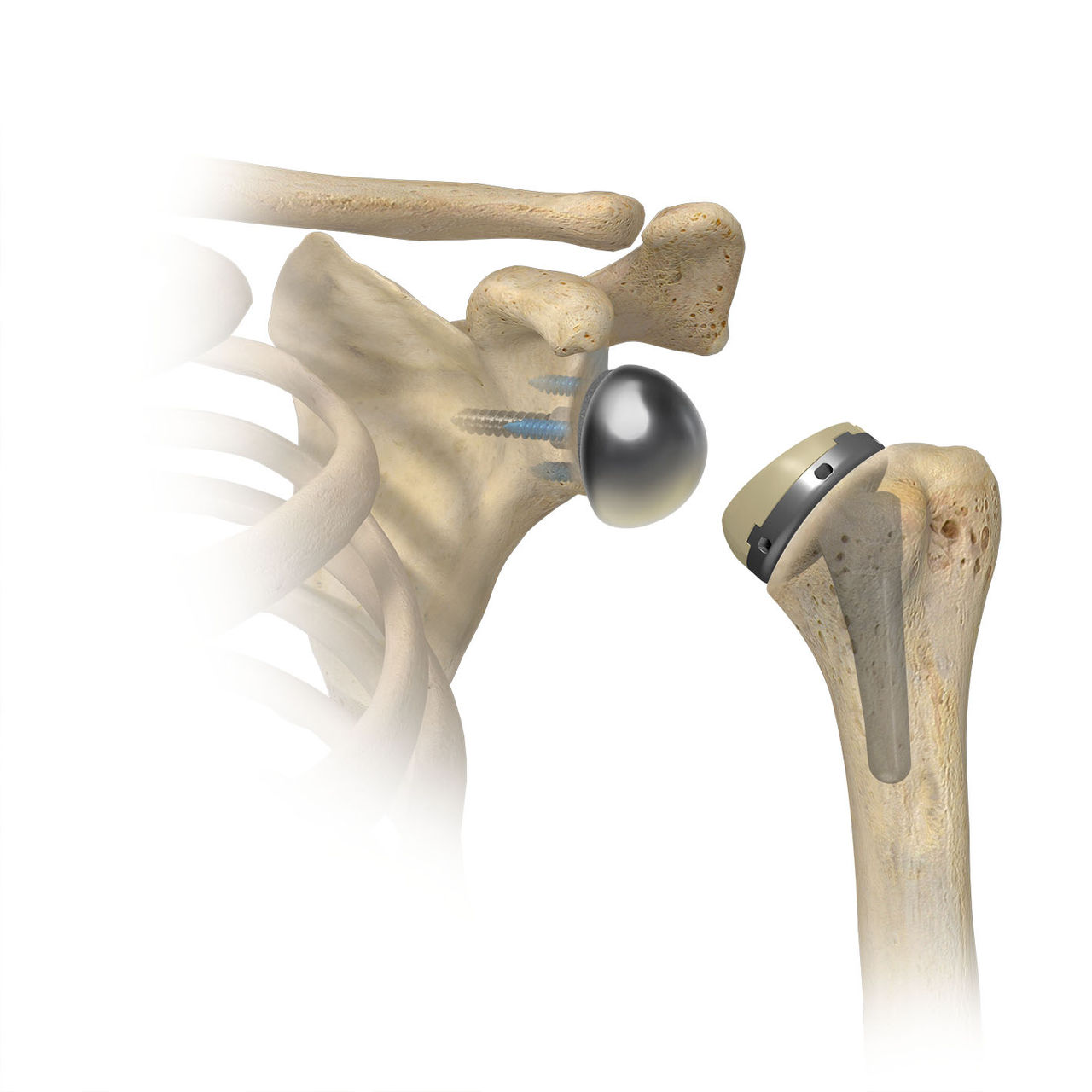
On the humeral (arm bone) side, a portion of the humeral head (ball) is removed and a metal stem is placed inside the bone. On top of this stem, a metal tray called a humeral adapter tray with a metal-grade plastic implant is placed. This is why we refer to this as a reverse system… the ball is now where the cup used to be and the cup is where the ball used to be.
A reverse shoulder replacement uses the outer muscle in your arm, the deltoid muscle, to power your shoulder. The implant typically lengthens the deltoid muscle. This helps compensate for an insufficient or torn rotator cuff.
There is an increasing use of reverse shoulder arthroplasty in the United States1, but both anatomic shoulders and reverse shoulders are intended for pain relief and improving function. The decision between each of these procedures is made based on multiple factors including status of the rotator cuff, the amount of remaining bone in the shoulder, pre-operative motion, age, and overall surgeon preference.
It’s helpful to discuss which of these procedures you may be a candidate for with your surgeon. In some cases, based on your specific diagnosis, your surgeon may have a good idea which procedure may be most appropriate. In other cases, the final decision between an anatomic shoulder replacement and a reverse shoulder replacement may be made at the time of surgery once the surgeon is able to fully see your joint.
Both anatomic and reverse shoulder replacements can help provide significant pain relief and improvement in function, for many patients. Along with greater awareness of the benefits of these procedures, evolving technology in instruments and implants, shoulder arthroplasty is growing significantly worldwide.1 Talk to your doctor to see if shoulder replacement might be an option for you and about the potential associated risks.